By Janet Fabbri – Musculoskeletal Physiotherapist
(Williams & Cohen 2009)
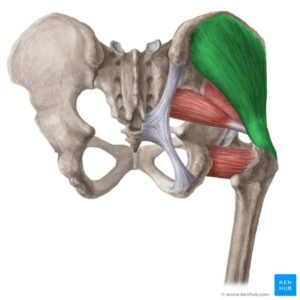
Gluteus Medius tendinopathy (affecting the common tendon of your gluteus medius (in green above) and gluteus minimus (in red), which is the connective tissue that connects the muscle to the bone . Tendinopathy is a degeneration/ tear within the tendon. Tears are not always painful, so having a scan is not necessary initially, and are only usually recommended if you are not improving after a few months.
Tendons do not like change – therefore they will not like a rapid increase in exercise or activity (e.g. a long day out, shopping or sitting in the car travelling to Sydney). They will not like too much rest either. Tendons need a similar amount of activity each day. They need consistent load.
Common Symptoms
- morning stiffness and pain (worst in the morning),
- night pain and you may have difficulty sleeping on your painful side,
- pain that seems to ease after you have started exercise (ie once you warm up),
- pain that is worse after activity such as walking, stairs, getting up from sitting or from the car.
Recovering from a tendinopathy requires consistent management over 3 months and can take approximately 12-18 months to recover completely and return to full function/sport.
Don’t start any new activity you haven’t tried for a while or persist with activities that increase/aggravate pain (check with your Physiotherapist first).
Risk Factors
- Age >40 years
- Female gender, especially with wider hips
- Menopausal/post-menopause
- Type 2 Diabetes
- High Cholesterol
- High blood pressure
- Higher levels of body fat
- Other systemic/metabolic conditions
- Recent antibiotics (Floroquinolones)
What not to do ❌
- Don’t rest it too much , keep gently moving. Don’t sit or stand or stay in one position for too long ( no longer than 10 -20 minutes in one static position, depending on the severity)
- Do not compress the tendon such as lying on your side it in bed, or if it is the higher hip when lying on your side in bed then place a pillow between your legs so that your knees are not close together. By reducing the stretch on the tendon it is not then compressed against the bone.
- Do not Stretch your hip muscles (ie in a crossing your legs position). This stretches the tendon over the bone which compresses it and this hurts as well as delaying healing.
- Do not Stand w one hip stuck out to the side (you need to stand with even weight in both legs)
- Do not do excessive amounts of walking or running. Limit walking up/down hills or stairs.
- Do not start any new activity you haven’t tried for a while,
- Do not use certain Anti-inflammatory medications (NSAIDs – see our ‘Insight’ about this) as they can be detrimental to tendon repair. (discuss use of these medications with your GP or Pharmacist).
- Do not eat bad food! Good nutrition is important for optimal tissue healing. Some food, such as sugars (including alcohol), increases inflammation so you will feel more pain and reduce healing of the tendon.
Your Physio will advise you about all of these things.
What to do ✅
- Consistent and progressive load is key in any tendinopathy.
- Observe and note what increases your pain (immediately and up to 72hrs after) and what eases your pain.
- Monitor your morning stiffness and night pain.
- Perform exercises as directed by your Physiotherapist or Exercise Physiologist (no more, no less). These will initially be:
- static holds of the Gluteus Medius Muscle for many seconds, repeated many times a day, to reduce pain, and
- heavy slow resistance of the Gluteus Medius Muscle using theraband.
- If you sleep side lying, place a pillow between your knees and ankles.
- Recommended methods for pain relief include:
- Ice
- Isometric (static) exercise within pain limits (25% of max effort)
- Self massage with a tennis ball to buttock muscles
- Regular use of Ibuprofen or Naproxen (discuss use of these medications with your GP or Pharmacist), however be aware that some of these may reduce healing.
If your pain is getting worse, it means the muscle/tendon is not coping with the load you have placed on it. If it is less stiff and sore, this is a good sign that your tendon is recovering, so keep maintaining the same amount of regular load. Pace yourself! If your hip hurts when walking or sitting for 30 minutes, you need to decrease it to 20 minutes. Avoid doing too much activity (racing about) in one day.
Book with one of our Physiotherapists to comprehensively assess you and to guide and progress your program. Tendinopathies generally take around 4 months to improve but this can be longer, even up to 12-18 months.


