Andrea Rich & Janet Fabbri – Physiotherapists
The Achilles tendon can be a commonly sore area in people that run and Achilles tendinopathy is one of the most common injuries of the foot and ankle.

What is Achilles Tendinopathy?
The Achilles tendon is the thick, tough fibre that connects your calf muscle to your heel. A tendon injury can occur due to
a) too much load too soon or
b) existing muscle weakness placing increased demand on the muscle and tendon.
If the load we put through a tendon is too much and we continue to load it without enough rest, the tendon doesn’t have enough time to repair. This leads to the structure of the tendon changing (called tendinopathy) and it is harder for the tendon to withstand loads. Often these loads are from repetitive movements such as running and jumping.
Should I be concerned if I want to start a new running program?
Lagas et al, 2019 researched the incidence of Achilles tendinopathy and the associated risk factors in recreational runners. They found that there is an increased incidence of Achilles tendinopathy in runners registering for 5-42km events and that the injury occurred on average 2 weeks before the event. They identified 3 risk factors for developing this injury in this demographic:
- A previous Achilles tendinopathy
- Chronic tendinopathies can take longer to heal and can still be changing even when you feel no pain. It is important to follow through with rehabilitation of a tendon injury after it feels better.
- To reduce relapse of injury it is recommended to participate in a maintenance rehabilitation program whilst also training for an event.
- Use of compression socks
- Identifying the reason for wearing compression socks is important and was found that runners were wearing them to try manage previous injury without knowing that they would be detrimental to an achilles tendiopathy.
- Often tendinopathies don’t like compression from things like muscle stretching or compression garments.
- Use of a training schedule
- It takes time to build up the strength and capacity of soft tissues (muscles and tendon). Training schedules are usually not individualised, and it was found that standard programs increased in volume and intensity too rapidly which didn’t allow enough time for tendons and muscles to adapt to the new load.
- New activities or increasing an activity must be properly graded and paced and your physio can help you do this at an individual level.
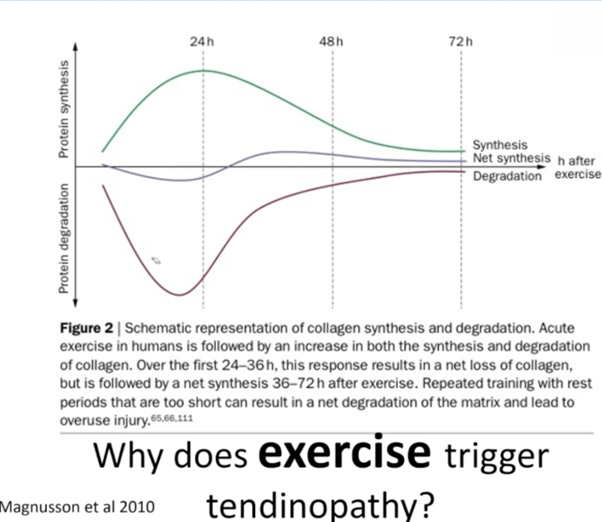
The Graph below by, Magnusson et al, shows why you must have a rest day between strength training so that enough time is allowed for the tendon to break down (about 24 hours) and then it will rebuild stronger tendon. If you train hard every day there will be a continual degeneration of the tendon and poor or no recovery.
If the tendon is not recovering and becoming chronic, then another treatment to consider is extracorporeal shockwave therapy for noninsertional ( i.e. not close to the heel bone) Achilles tendinopathy. A recent randomised controlled trial with Level 1 evidence done on people with chronic achilles tendinopathy showed that combining calf eccentric loading with stretching exercises resulted in significant improvements in the pain and function. Adding ESWT to this combined protocol resulted in significantly greater improvements in both the short and long term.
What not to do ❌
- Do not stretch your calves in the early phases (especially if an insertional tendinopathy i.e pain at the heel insertion point), so walking or running up (or down) hills and stairs can do this – you may need to run less on your heels and even walk with a heel raise in your shoes. (See your Physio to advise)
- Avoid standing calf stretch with hands on wall and heel back – this compresses the injured tendon against the bone, reduces blood supply, reduces healing, and increases pain.
- Do not sit for too long (you can sit – just make sure you move your ankle),
- Do not start any new activity you haven’t tried for a while,
- Do not do over the step calf raises (for an insertional tendinopathy) initially, but gradually you will progress to doing these.
- Do not have a Steroid injection– corticosteroids can impair collage synthesis and reduce the tensile strength of a tendon (Scott et al. 2015). Long term use of steroids may increase risk of rupture, especially following tendon injection.
- Do not use certain anti-inflammatory medications (NSAIDs – see our ‘Insight’ about this) as they can be detrimental to tendon repair.
- Do not eat bad food! Good nutrition is important for optimal tissue healing. Some food, such as sugars (including alcohol), increases inflammation so you will feel more pain.
If you are a recreational runner with previous injuries thinking about registering for an event, contact us for more information on how to reduce your risk of overuse injury by correctly managing your training program.
See one of our physiotherapists to comprehensively assess you and to guide and progress your program. Tendinopathies generally take around 4 months to improve but this can be longer, even up to 12-18 months.
Our Reformer and Matwork classes , or specific individually designed gym sessions, using our Pilates equipment can help to strengthen and stabilise the ankle region and lower body for optimal recovery. Speak to your Physio about which class would suit you.
References:
Lagas et al, 2019
Abdelkader NA, Helmy MNK, Fayaz NA, Saweeres ESB. Short- and intermediate-term results of extracorporeal shockwave therapy for noninsertional Achilles tendinopathy. Foot & Ankle International, 2021 Jan 15. Epub ahead of print. Clinical trial