By Janet Fabbri – Musculoskeletal Physiotherapist
What is Sciatica?
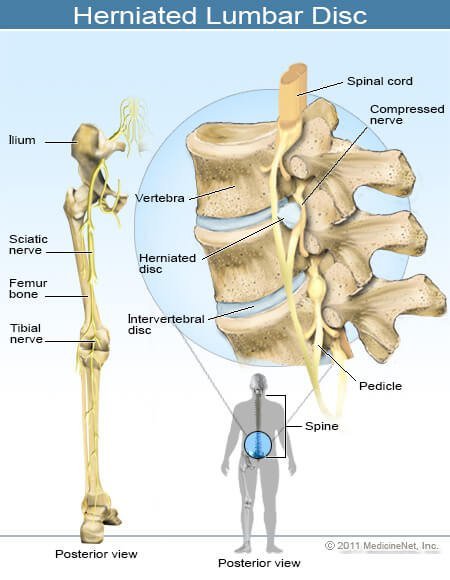
“Sciatica”, also known as “nerve root compression” or “lumbar radiculopathy” is leg pain (burning, sharp shooting, achy, deep, or “ nervy”), weakness, numbness and/or pins and needles caused by the compression of a nerve in the spine. Usually caused due to a disc bulge, but can also be from neighbouring bone such as with severe osteoarthritis, a spondylolisthesis ( a vertebra that has slipped forward relative to the vertebra below it), or even from a cyst. The nerve root exits the spine at the “intervertebral foramen” (or “hole between the spinal vertebrae -in Latin”) and then joins other nerve roots to form a nerve. The Sciatic nerve is made up of the nerve roots from L4 to S1 in the lower lumbar spine:
Pain will only occur when there is compression on a nerve root that is “pre- sensitised” by chemicals called cytokines, that can be released from a disc bulge or prolapse. Normal nerves cope very well with being compressed and in normal function our nerves get compressed (and stretched) a lot all over the body. Compression plus chemical irritation leads to reduced blood supply to the nerve root and some loss of nerve function (less power to the muscles, pain which is perceived to come from the leg, and reduced sensation – numbness) which can take a long time to recover from, sometimes taking 6 to 18 months or longer. This “Neuroinflammation” can even spread, and the central nervous system (spinal cord and brain,) can then make this better or worse over time ( See our ‘Insight’ about “Pain”). It is extremely complex.
Known risk factors of Sciatica are:
- Smoking
- Obesity
- Manual work, repetitive and loaded bending
- Driving a lot
- Poor job satisfaction and mental stress
- Moderate walking ( which ironically is also one of the treatments for this condition – if you have a biomechanical issue that needs to be corrected, then Physio can identify and guide you with this and then optimal , paced walking can help).
Diagnosis
Correct diagnosis of sciatica is essential, because there are other causes of leg pain that will be treated differently to sciatica. These other “ differential” diagnoses are :
- “Referred leg pain” from a joint in the lumbar spine, which occurs because the brain interprets pain coming from a back structure as pain coming from the area supplied by nerves at that same spinal level, so treatment usually requires mobilisation of the lumbar joint/s, and has nothing to do with reducing the compression on the nerve, because the nerve is not compressed. Referred leg pain is very common. The pain is felt in a different place to where it is coming from. An example of this is Angina, where heart problems are felt in the left arm or throat or chest or back.
- Spinal canal stenosis, which is usually worse with extension and better with flexion.
- Peripheral Artery disease, also called intermittent claudication, which requires medical attention. Usually it comes on with walking, and is relieved immediately by rest.
- Meralgia Paraesthetica , which is a peripheral nerve entrapment of the lateral femoral cutaneous nerve. There are other peripheral neuropathies, such as Tarsal Tunnel syndrome in the foot.
- Greater trochanteric pain Syndrome, or Gluteus Medius tendinopathy
- Hip osteoarthritis and Avascular necrosis
- SIJ Dysfunction
- Piriformis/Deep gluteal Syndrome
- Inflammatory / Metabolic Disorders
Do I need a scan?
Sciatica initially does not need to have a scan , such as MRI but later may be needed if surgery is contemplated ( if your symptoms are ongoing and severe, or the neurological deficit is worsening). The diagnosis is based on Signs and symptoms which your Physio will determine in the clinical examination.
Treatment for sciatica
- Exercise, in particular different types of supervised exercise.
– Core stability -Most people with this condition have a lot of spasm in their lumbar spine muscles which are acting to brace the area ( subconsciously) and the “core” becomes weak ( see our ‘Insight” about “ Core Stability”) so targeted exercises to improve core stability can help.
-Back flexibility exercises, in particular back extensions ( such as McKenzie exercises) and often rotation and side bending are prescribed to in specific ways to take the load off the pinched nerve and to return the spine to more normal biomechanical load.
-Strength of the back and the rest of the body can aid recovery and also prevent further deconditioning.
-Endurance– Cardiovascular fitness needs to be done according to the World Health Organisations guidelines of 150 minutes a week of moderate exercise, such as walking, however, this needs to be paced so that your condition is not aggravated.
Our Physiotherapists specifically diagnose and provide you with the appropriate specific exercise program that should be done very regularly , usually a few times a day , if you are in severe pain. You can also do an individualised Gym session on our Pilates equipment on your own that can be very beneficial. If your condition is not too sever than joining one of our Clinical Exercise classes ( reformer / Matwork) is recommended. Your Physio will advise on this.
- Manual therapy from your Physio, which in my clinical experience, is essential , especially reducing the stiffness of the joints in the thoracic spine (mid spine where the ribs join) , which are often very stiff. This is usually done over a few sessions and research has shown that it should not go on for a long time (months) because you can become dependent on passive treatment and not do exercises, that have been shown to be very effective.
- Lumbar spine traction. Evidence in the past has been controversial but support for traction has only recently been shown to be effective. The literature suggests that, for pain and disability in lumbar radiculopathy, there is short-term effectiveness of supine mechanical traction when added to physiotherapy intervention. Other studies have shown that traction is no more effective than other treatments ( mentioned above)
- Education about prognosis to help you understand that it can take a long time (can be many months), and knowing that 2/3 of disc lesions repair on their own!
- Education about Pacing your activities. This avoids “fear avoidance behaviour” which can gradually make you less and less active and worsen your pain. We will help you to find your Baseline of activity and show you how to incorporate this into your life.
- Advice to remain active and do your usual activities within reason, and to limit resting to only 10-20 minutes at a time, so not staying in bed all day, which makes your pain worse and leads to depression. Walking is a good activity, and so is swimming.
- Advice about warning signs, such as noticing more tingling in your lower leg can be a sign that you have overloaded the nerve in the spine. You need to know what activities can make your pain worse, which may be heavy lifting, prolonged sitting so this should be done in a paced way , rather than avoiding it altogether.
- Acupuncture and dry needling is NOT Neither are passive treatments such as hot packs/ ice. It is better to spend this time doing your exercises!
- Medications and injections are not recommended, but short term use of some may be needed to enable you to do get through your day and do your exercises! If you are not improving or worsening speak to your Doctor. The use of injections is controversial.
- Surgery should be done as a last resort, but this has been proven to be effective for the relevant cases, when conservative treatment has failed. A recent randomised controlled trial showed that sixty percent of patients with sciatica who had failed other medical management benefited from spinal manipulation to the same degree as if they underwent surgical intervention. Of 40% left unsatisfied, subsequent surgical intervention confers excellent outcome. It was recommended that Patients with symptomatic sciatica failing medical management should consider spinal manipulation followed by surgery if warranted.
However, the results about surgery are not always clear. A recent trial Surgical versus nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial, patients in both the surgery and the nonoperative treatment groups improved substantially over a 2-year period. Because of the large numbers of patients who crossed over in both directions, conclusions about the superiority or equivalence of the treatments are not warranted based on the intent-to-treat analysis.
High quality research is lacking in the area of surgery versus other interventions, but it is recommended to try conservative (non surgical) options first.
References
Murry. L from Physio Network: Differential Diagnosis of Radicular Pain.
Stochkendahl. M.J, Kjaer.P, Hartvigsen.J, Kongsted. A, Aaboe. J, Andersen. M, Andersen. M, Fournier. G, Hojgaard. B, Jensen. M.B, Jensen. L. D, Karbo. T, Kirksekov. L, Melbye. M, Morsel-Carlsen. L, Nordsteen. J, Skuli Palsson. T, Rasti. Z, Frost Silbye. P, Zebitz Steiness. M, Tarp. S, Vaagholt. M (2018) National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. European Spine Journal, Vol. 27, Pg 60-75
Vanti C, Panizzolo A, Turone L, Guccione AA, Violante FS, Pillastrini P, Bertozzi L (2020), Effectiveness of mechanical traction for lumbar radiculopathy: A systematic review and meta-analysis. Physical Therapy
Schimmel. J, Kleuver. M. de, Horsting. P.P, Spruit. M, Jacobs. W.C.H, Van Limbeek. J (2009) No effect of traction in patients with low back pain: a single centre, single blind, randomized controlled trial of Intervertebral Differential Dynamics Therapy. European Spine Journal, Vol.18, Article number: 1843
Zhong M, Liu JT, Jiang H, Mo W, Yu PF, Li XC, Xue RR. Incidence of Spontaneous Resorption of Lumbar Disc Herniation: A Meta-Analysis. Pain Physician. 2017 Jan-Feb;20(1):E45-E52. PMID: 28072796.
McMorland G, Suter E, Casha S, du Plessis SJ, Hurlbert RJ (2010) Manipulation or microdiskectomy for sciatica? A prospective randomized clinical study. Journal of Manipulative and Physiological Therapeutics 2010 Oct;33(8):576-584
Weinstein JN, Tosteson TD, Lurie JD, Tosteson ANA, Hanscom B, Skinner JS, Abdu WA, Hilibrand AS, Boden SD, Deyo RA (2006) Surgical versus nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA 2006 Nov 22;296(20):2441-2450
Fernandez, M Ferreira, M.L., Refshauge, K.M., Hartvigsen, J., Silva, I.R.C., Maher, C. G., Koes, B.W., Ferreira, P.H. Surgery or physical activity in the management of sciatica: a systematic review and meta-analysis. European Spine Journal, Vol 25, pg3495-3512 ( 2016).


